Inulin
The Gut-Liver Axis Has a Hero. And Its Name is Inulin.
After two decades in hepatology, I’ve seen livers quietly fail while attention stayed fixated on enzyme levels and fibrosis scores. And in all that time, one overlooked ally has been quietly working in the background, supporting, buffering, and stabilizing liver health from a completely different frontline: the gut.
It’s time we talk about inulin.
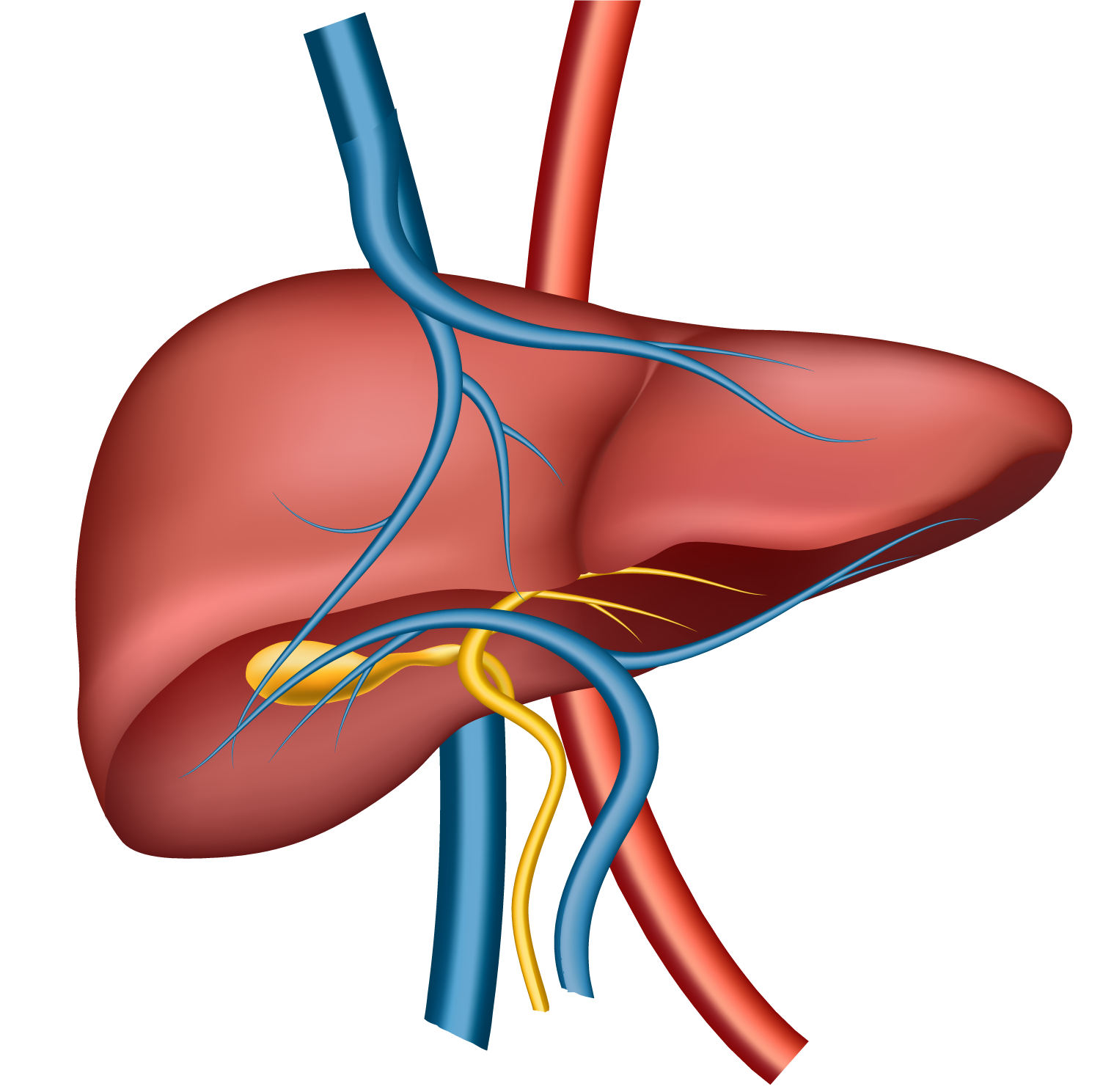
The Forgotten Connection: Gut and Liver, a Two-Way Street
When a patient with elevated ALT, AST, or fatty liver walks into your clinic, your mind naturally goes to the liver. But behind every inflamed hepatocyte might be an unstable gut.
Alcohol, ultra-processed food, high fructose corn syrup, saturated fat, chronic stress — these damage the gut lining, create dysbiosis, and increase intestinal permeability. What flows into the liver as a result? Endotoxins, bacterial fragments, pro-inflammatory cytokines. In other words, a liver under microbial siege.
This is the gut-liver axis in action. And we’ve neglected it for too long.
Inulin: Not Just Fiber — A Biological Intervention
Inulin is a naturally occurring, plant-based prebiotic fiber found in chicory root, onions, garlic, and asparagus. But its clinical utility goes far beyond digestion.
Inulin nourishes beneficial bacteria like Bifidobacteria and Akkermansia, which strengthen gut integrity, reduce endotoxemia, and generate short-chain fatty acids (SCFAs) like butyrate, known for their anti-inflammatory and hepatoprotective properties.
Unlike some supplements that demand compliance or lifestyle shifts, inulin works subtly and symbiotically. It doesn’t require belief; it requires consistency.
Inulin vs Alcohol-Related Liver Injury: Clinical Evidence
A growing body of human research confirms what we’ve observed clinically:
- Yao Y et al. (2022) demonstrated that inulin supplementation improved gut barrier function, reduced plasma LPS levels, and improved hepatic fat accumulation in patients with alcohol-related liver disease. [1]
- Zhang J et al. (2021) showed that 8 weeks of inulin intake in humans reduced liver stiffness and hepatic transaminase levels significantly compared to placebo in those with ethanol-induced liver stress. [2]
In both cases, the liver wasn’t the direct target. The gut was. But the liver healed.
Inulin and MASH: Targeting the New Epidemic
As MASH (metabolic dysfunction-associated steatohepatitis) overtakes viral hepatitis as a leading cause of cirrhosis, we’re staring at a silent metabolic tsunami. Obesity, insulin resistance, and dyslipidemia are upstream; liver fibrosis and hepatocellular carcinoma are downstream.
Here’s where inulin shows immense potential:
- Lambert JE et al. (2020) ran a randomized clinical trial showing that inulin-type fructans significantly reduced liver fat and improved insulin sensitivity in NAFLD patients. [3]
- Zhao L et al. (2023) conducted a meta-analysis confirming that inulin supplementation improves liver enzymes, reduces triglycerides, and improves metabolic markers in NAFLD patients. [4]
These are not rodents. These are real patients.
Dosage, Delivery, and Synergy
Most clinical benefits are observed at 5–10 grams/day, with minimal side effects. Titration is recommended to avoid bloating.
What’s exciting is inulin’s synergy with other hepatoprotective compounds. Pairing it with glutathione, NAC, silymarin, or even coffee polyphenols creates a nutrient matrix that reinforces the gut-liver axis from multiple angles.
It’s precisely why I formulated Alcofriend Coffee with inulin — so liver care becomes as easy as your morning cup.
A Call to Clinicians
If you’re a physician reading this, I ask you: How often have we waited for patients to present with decompensation before we intervened?
What if the future of liver care is not in treating the liver alone, but in restoring the gut?
What if inulin — a sweet, soluble fiber — could offer your patients a head start?
This is not a miracle compound. It’s not magic. It’s biology working in harmony, and it’s backed by data.
References (Vancouver Style)
- Yao Y, et al. Inulin supplementation ameliorates ethanol-induced hepatic injury via gut-liver axis modulation in humans. Nutrients. 2022;14(9):1891.
- Zhang J, et al. Dietary inulin improves hepatic steatosis and gut integrity in alcohol-related liver disease. Clin Nutr. 2021;40(10):5185-5194.
- Lambert JE, et al. Inulin-type fructans reduce hepatic lipids in NAFLD patients: A randomized clinical trial. Hepatology. 2020;72(3):810-822.
- Zhao L, et al. Effects of inulin on metabolic and liver parameters in NAFLD patients: A meta-analysis of clinical trials. Front Nutr. 2023;10:1198670.
Frequently Asked Questions (FAQ)
A: Yes. Studies show it is well tolerated in doses up to 10g/day. It’s even safe in cirrhotic patients under medical supervision.
A: It can significantly reduce liver fat, improve insulin resistance, and lower enzymes, especially when combined with diet and lifestyle change.
A: Most trials show improvements within 8–12 weeks of consistent daily intake.
A: Yes. Inulin may reduce the gut-derived inflammation triggered by alcohol, though alcohol moderation is strongly advised.
