How Alcohol Damages Liver
Alcohol Effect on Liver - Mechanism
Alcohol Absorption and Transport to the Liver
Ingestion and Absorption:
After consuming alcohol, it passes through the esophagus to the stomach and small intestine. Approximately 20% of alcohol is absorbed in the stomach, while the remaining 80% is absorbed in the small intestine. Alcohol absorption is rapid, particularly on an empty stomach.Transport Through Blood:
Absorbed alcohol enters the bloodstream via the intestinal capillaries. Through the portal vein, it is transported directly to the liver, the primary site for alcohol metabolism.

Alcohol Entry into Liver Cells
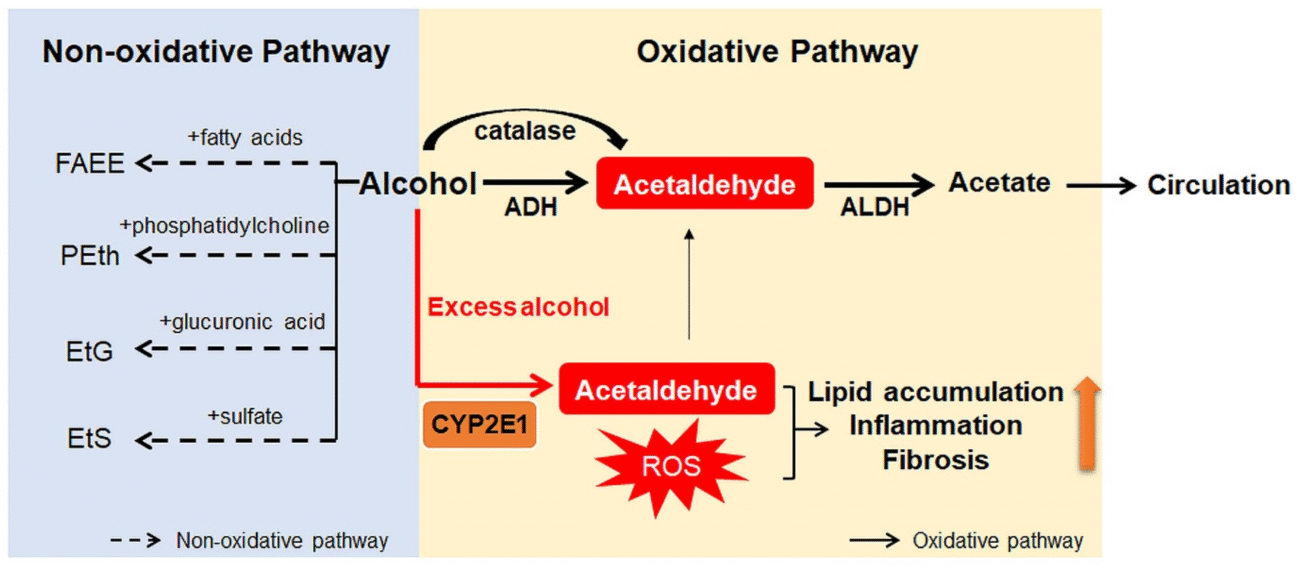
- Once in the liver, alcohol enters hepatocytes (liver cells) where it is metabolized primarily by:
- Alcohol Dehydrogenase (ADH): Converts alcohol to acetaldehyde, a toxic and reactive compound.
- Cytochrome P450 2E1 (CYP2E1): Induced by chronic alcohol consumption, it produces reactive oxygen species (ROS) alongside acetaldehyde.
- Catalase: Plays a minor role in alcohol metabolism.
Mechanisms of Alcohol-Induced Liver Damage
- Acetaldehyde Toxicity:
- Acetaldehyde binds to proteins and DNA, forming adducts that impair cell functions and trigger immune responses.
- It disrupts mitochondrial function and induces oxidative stress.
- Oxidative Stress:
- Alcohol metabolism generates excessive ROS, which damage lipids, proteins, and DNA in hepatocytes.
- Lipid peroxidation weakens cell membranes, making cells more prone to injury and death.
- Gut-Liver Axis Dysfunction:
- Alcohol disrupts gut barrier integrity, allowing endotoxins (e.g., lipopolysaccharides) to enter the bloodstream and reach the liver.
- Endotoxins activate Kupffer cells (liver macrophages), leading to inflammation and release of pro-inflammatory cytokines.
- Fatty Liver Formation (Steatosis):
- Alcohol impairs lipid metabolism, increasing triglyceride synthesis and reducing lipid export from hepatocytes.
- This leads to the accumulation of fat in liver cells, causing alcoholic fatty liver disease (AFLD).
Progression to Liver Scarring and Cirrhosis
- Inflammation and Hepatocyte Death:
- Persistent alcohol consumption causes ongoing inflammation and hepatocyte apoptosis (programmed cell death) or necrosis.
- Fibrosis (Liver Scarring):
- Activated hepatic stellate cells produce excessive collagen and extracellular matrix proteins in response to chronic injury and inflammation.
- This scarring disrupts normal liver architecture and blood flow.
- Cirrhosis:
- Advanced scarring leads to liver cirrhosis, characterized by:
- Irreversible fibrosis.
- Loss of functional liver tissue.
- Complications like portal hypertension, ascites, and liver failure.
- Advanced scarring leads to liver cirrhosis, characterized by:
Conclusion
Alcohol’s journey from ingestion to liver damage is a complex process involving absorption, metabolism, and cascading cellular injuries. Early-stage damage, such as fatty liver, is often reversible with abstinence and lifestyle changes. However, continued alcohol consumption leads to progressive scarring and cirrhosis, which is irreversible and life-threatening.